Blocked (Plugged or Clogged) Milk Duct Education Series, Part 2: Home & In-Clinic Treatment Options for Blocked Ducts
Blocked (Plugged or Clogged) Milk Duct Education Series: Part 2 of 3.
Home & In-Clinic Treatment Options for Blocked Ducts & Mastitis

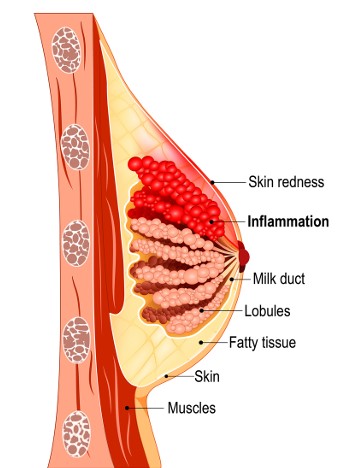
If you suspect you have a clogged duct, and especially if you think you have mastitis, you should contact your health care provider to let them know. They will ask you some screening questions to determine the urgency of your case.

One treatment I offer that has helped hundreds of women is a painless and comforting treatment called Therapeutic Ultrasound. In most cases, the duct can be unblocked in 1-2 sessions. This is an evidenced-based treatment that is often recommended by maternity care providers in Squamish, who refer their patients to me for this treatment. I can also add therapeutic cupping, as well as acupuncture (with or without microcurrent/MPS), to further enhance the treatment.
What can you do to get started right now? :
Brigham and Women’s Hospital Standard of Care states that “Ultrasound has been shown to be of benefit in the treatment of blocked milk ducts.”
La Leche League offers the following advice when you suspect a clogged duct:
- Breastfeed as often as your baby wishes
- Rest
- Apply ice or cold packs to the tender area
- If you are engorged, consider doing lymphatic drainage—a very gentle, light yet firm touch, with fingertips flat to the skin in the armpit area and upper chest. To see a demonstration of lymphatic drainage massage, you can watch this video
- In consultation with your healthcare provider, consider using ibuprofen (Advil®) alternating with acetaminophen (Tylenol®)
There is also a supplement called lecithin (available at Nesters in the Wellness Department) which is often prescribed to women with blocked ducts. Brigham and Women’s Hospital’s Standard of Care states that “the milk secretions that remain in the breast from blocked ducts have a very high fatty composition with a higher rate of absorption. Lecithin is a phospholipid emulsifier and can be used to emulsify milk secretions to promote breast emptying. The typical dosage is 1200 mg/day 3-4 times per day.“ Please speak with your medical team regarding any supplements.
Hydrate more than usual and rest when you can!
In writing this blog post, I learned that some common advice is now OUTDATED!
La Leche League updated their post on this topic in 2023 to say that the following strategies are NO LONGER recommended:
Heat to the breast, or soaking in warm waterVigorous, deep massage, or squeezing to try to get rid of a clogDangling over baby for feeding to try to move a clog using gravityUsing a comb, vibrator, or electric toothbrush on the breastTrying to “empty” the breast through extra pumping or breastfeeding which increases milk productionUsing antibiotics right at the beginning of symptomsUsing Epsom salts in a Haakaa or similar silicone breast pump for nipple blebsUsing saline soaks, warm compresses, olive oil, castor oil, or other oils on the skin of the breast or nippleRemoving the skin or “popping” a bleb, which may allow infection to develop- Routine sterilization of pumps and household items is not necessary, although daily cleaning according to the manufacturer’s instructions is important to avoid infection from dirty pump parts.3 For more general information see this fact sheet.
My next post will outline evidence-based tips on how to prevent mastitis:
As mentioned previously, in Squamish, we are fortunate to have an exceptional group of practitioners to help with lactation questions, including the new collaboration between Mountain Maternity and Roots Midwives, and Anna Turyk of Nuture Sea To Sky Lactation Consulting Services. La Leche League Squamish is also an excellent resource.
Strategies to treat and prevent clogged ducts, including treatments I offer in the clinic, are coming up in the next post!