Introducing the Slinky Spine class with Kinesiologist Mel Sakowski
Below is a guest post from Kinesiologist Melanie Sakowski!
Hi, I’m Kinesiologist on the Union Team and I’m so grateful to be welcomed to the team!
Coming from Toronto after completing my undergraduate degree in Kinesiology, I
transitioned from triathlon to trail running, and am passionate about movement patterning,
rhythm and fluidity in movement. My passion is to help someone learn and understand their
movement, to feel connection from feet through head dynamically as they move through life!
I am fascinated by the creative art of movement, and how mind-body connection interplays.
My Slinky Spine class offered at Union Health and Performance focuses on relieving neural
and dural tension in the body.
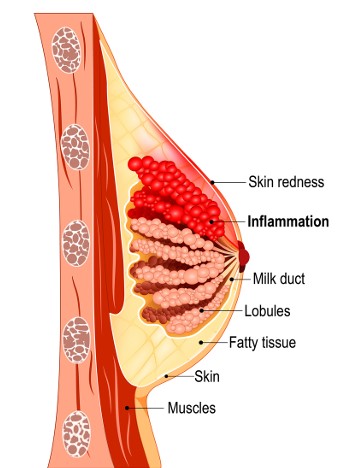
The Dura Mater, or the “Tough Mother”, is a thick lining of the spinal cord and brain. Tensions
developed from within the cranial dura mater can transmit through the innervations along the
spinal cord and through the nerves down from the cranium to the sacrum. This tension can
restrict blood flow to the nerves, and cause different symptoms in the body that might distort
movement patterns, breathing, and emotional states. There might be a sensation of having
a specific holding pattern in the body that presents itself during periods of high stress or any
change in your life. Nerves in the body cannot be stretched, they glide and slide. When a
nerve is compressed, the body will protect the nerve by contracting around that compressed
nerve. The nervous system tries to protect itself first and foremost!
These nerve compressions could cause distortions that could present in different holding
patterns on body tissues, and sensations like numbness, tingling or physical symptoms that
seem to be unresolvable through traditional strengthening, stretching, mobility approaches or
manual therapies.
Nerves can get compressed from a myriad of different ways; physical traumas, high levels of
stress, neurological conditions, excessive sitting or staying in certain positions for prolonged
periods of time, spinal disc injuries, bony injuries or shape changes (osteoarthritis, bone
spurs), scar tissue formation or adhesions that can stick to nerves, or acute injuries causing
swelling.
Because the body contracts in twisting patterns, if there’s a tension, there will be a twist
pattern of contraction. Relieving tension allows the spine to unwind and unravel back to a
more balanced place for each body in their most organic way.
Give these a try!
https://www.youtube.com/watch?v=Hb3xxH2vRcU
Tight adductors and the line of tension from the shoulder running diagonally across the body
to the opposite knee is one that might get tight and restrict movement freedom, so this
mobilisation pairs breath to lengthen the line of the hip flexor, through the psoas and
accessory breathing muscles and to open the shoulder allowing for expansion in the front of
the body and extension in the back.
https://www.youtube.com/watch?v=r0K1lFsLyJA
This nerve floss, the “Egyptian”, invites the nerves through the opposite arm through
opposite foot to glide and slide: if you think of a towel that is twisted around a string, if you
twist the towel more, the string will be asked to slide and glide against the towel. So this
nerve floss, pressing hips-to-heels-to heart-to-hand gives the nerves space to move along
the line from foot to hand. This is a fun one to play with in your body by being creative with
your shape and how you feel like expressing yourself from your inside.
Colntact Melanie Sakowski at melaniesakowski999@gmail.com or 1-(250) 650-5771
Instagram @wildkinesiology
Slinky Spine takes place Tuesdays 3-4pm at Union Health and Performance:
https://unionhealthandperformance.janeapp.com/#/staff_member/21